Pain nursing care plans are essential for addressing patient discomfort‚ promoting comfort‚ and enhancing quality of life. Customizable PDF templates simplify documentation‚ ensuring tailored‚ effective care for diverse needs. These plans guide holistic approaches‚ fostering consistency and better patient outcomes through structured assessments and interventions. They serve as valuable tools for nurses to deliver compassionate‚ evidence-based pain management.
1.1 Importance of Nursing Care Plans in Pain Management
Nursing care plans are vital for effective pain management‚ ensuring personalized‚ patient-centered approaches. They guide tailored interventions‚ improving consistency and outcomes. By documenting assessments‚ goals‚ and interventions‚ these plans enhance communication among healthcare teams. Standardized templates‚ like PDF formats‚ streamline documentation‚ reducing errors and saving time. They also ensure legal and ethical compliance‚ protecting both patients and providers. Care plans empower nurses to address diverse pain experiences‚ from acute to chronic‚ using evidence-based practices. Regular updates and patient feedback refine these plans‚ optimizing care quality. Ultimately‚ nursing care plans are foundational for delivering compassionate‚ efficient‚ and effective pain management‚ fostering better patient satisfaction and recovery.
1.2 Overview of Pain Assessment and Documentation
Pain assessment and documentation are critical steps in creating effective nursing care plans. They involve evaluating the patient’s pain using standardized tools‚ such as the OLD CARTS framework‚ which assesses onset‚ location‚ duration‚ characteristics‚ aggravating factors‚ relieving factors‚ timing‚ and severity. Age-appropriate tools ensure accurate data collection for diverse patient populations. Documentation includes both subjective patient reports and objective observations‚ providing a comprehensive baseline for care. Accurate records help track progress‚ guide interventions‚ and communicate plans across healthcare teams. PDF templates streamline this process‚ offering organized formats for assessments‚ goals‚ and interventions. Proper documentation ensures continuity of care‚ legal compliance‚ and improved patient outcomes‚ making it a cornerstone of pain management nursing.
1.3 Benefits of Using PDF Templates for Pain Care Plans
PDF templates for pain care plans offer numerous benefits‚ including accessibility‚ customization‚ and consistency in documentation. They provide a structured format for assessing‚ planning‚ and tracking patient progress‚ ensuring all critical elements are addressed. Templates save time‚ reduce errors‚ and enhance organization‚ making it easier to share information among healthcare teams. They also allow for easy updates and adaptation to individual patient needs. Additionally‚ PDF templates promote professional presentation and compliance with legal standards‚ as they often include essential sections like goals‚ interventions‚ and outcomes. Their versatility makes them a valuable resource for nurses‚ enabling efficient and effective pain management care. Regular use of these templates improves documentation accuracy and supports high-quality patient care.

Assessment of Pain in Nursing Care
Assessing pain involves collecting subjective and objective data‚ using frameworks like OLD CARTS‚ and employing age-appropriate tools to guide personalized care plans effectively.
2.1 Subjective and Objective Data Collection
Effective pain assessment combines subjective and objective data to create a comprehensive understanding of a patient’s condition. Subjective data includes patient-reported information‚ such as pain intensity‚ description‚ and impact on daily activities. Objective data involves observable signs‚ like facial expressions‚ vital signs‚ and behavioral changes. Nurses use tools like the OLD CARTS framework to guide collection‚ ensuring thorough documentation. This dual approach helps formulate accurate diagnoses and tailored interventions. Age-appropriate assessment tools‚ such as pain rating scales or behavioral indicators‚ are essential for diverse patient populations. Accurate and detailed data collection is crucial for developing realistic care plans and evaluating progress. Proper documentation ensures continuity of care and informs future interventions.
2.2 Using OLD CARTS Framework for Pain Assessment
The OLD CARTS framework is a systematic approach to pain assessment‚ helping nurses gather comprehensive information. It stands for Onset‚ Location‚ Duration‚ Characteristics‚ Aggravating/Alleviating factors‚ Radiation‚ Timing‚ and Severity. This method ensures consistency and thoroughness in data collection. Nurses use it to identify patterns and understand the patient’s pain experience fully. By documenting each component‚ care plans become more patient-centered and effective. The framework aids in distinguishing acute from chronic pain and guides appropriate interventions. It also facilitates clear communication among healthcare team members. Regular use of OLD CARTS promotes accurate diagnoses and tailored treatment strategies‚ improving patient outcomes and satisfaction. This structured approach is invaluable for developing realistic and actionable care plans.
2.3 Age-Appropriate Pain Assessment Tools
Age-appropriate pain assessment tools are crucial for accurate pain evaluation across different patient populations. For pediatric patients‚ tools like the Wong-Baker Faces Pain Rating Scale or the FLACC scale are effective. Adults often use the Visual Analog Scale (VAS) or Numeric Rating Scale (NRS). Geriatric patients may require observational tools‚ such as the Pain Assessment in Advanced Dementia (PAINAD) scale‚ due to potential cognitive limitations. These tools ensure that pain assessment is tailored to the patient’s developmental and cognitive abilities‚ fostering reliable data collection. Incorporating these tools into care plans enhances the ability to create personalized interventions‚ leading to better pain management outcomes. They also promote consistency in documentation‚ aiding in the development of effective‚ patient-centered care strategies.

Nursing Diagnosis for Pain Management
Nursing diagnoses for pain management include acute and chronic pain‚ focusing on characteristics like intensity‚ onset‚ and impact on daily life. Patient-specific goals are established.
3.1 Acute Pain Diagnosis and Characteristics
Acute pain is characterized by sudden onset‚ short duration‚ and clear cause‚ often linked to tissue damage or surgery. It is typically sharp‚ localized‚ and resolves with healing. Nursing diagnoses focus on pain relief‚ addressing both verbal and non-verbal cues. Goals include reducing pain intensity within 3-4 hours and achieving pain-free status within 1-2 days. Baseline assessments guide realistic planning‚ considering patient-specific factors. Documentation ensures consistent‚ effective care‚ promoting comfort and preventing complications. Acute pain management is crucial for restoring function and improving patient outcomes‚ with interventions tailored to individual needs and responses. Early identification and intervention are key to successful acute pain care.

3;2 Chronic Pain Diagnosis and Considerations
Chronic pain is diagnosed when pain persists beyond the expected healing period‚ often exceeding three months. It can result from inflammation‚ nerve damage‚ or idiopathic causes. Assessment involves evaluating pain history‚ triggers‚ and impact on daily life. Nursing care plans for chronic pain focus on managing symptoms‚ improving function‚ and enhancing quality of life. Patient-specific goals are tailored to address long-term needs‚ incorporating both pharmacological and non-pharmacological interventions. Documentation of pain patterns and responses to treatments is crucial for ongoing care. Chronic pain management requires a holistic approach‚ addressing physical‚ emotional‚ and social factors. Nurses play a vital role in helping patients adapt to chronic pain and achieving realistic‚ patient-centered outcomes.
3.3 Identifying Patient-Specific Pain Goals
Patient-specific pain goals are tailored to address individual needs‚ ensuring realistic and achievable outcomes. These goals are developed in collaboration with the patient‚ focusing on improving function‚ reducing pain intensity‚ and enhancing quality of life. Nurses use pain assessment data to define measurable objectives‚ such as pain intensity levels‚ activity tolerance‚ and adherence to prescribed regimens. Goals are set using the SMART framework (Specific‚ Measurable‚ Achievable‚ Relevant‚ Timed). For example‚ a goal might be to “reduce pain from 8/10 to 4/10 within 48 hours.” Regular reassessment and documentation ensure progress is tracked‚ and goals are adjusted as needed. Patient involvement in goal-setting fosters empowerment and adherence to care plans‚ promoting effective pain management and improved well-being.
Goals and Objectives in Pain Nursing Care Plans
Pain nursing care plans establish specific‚ measurable goals to improve patient outcomes. These objectives are patient-centered‚ focusing on pain relief‚ functional improvement‚ and enhanced quality of life.
4.1 Setting Patient-Centered‚ Measurable‚ and Timed Goals
Setting patient-centered‚ measurable‚ and timed goals is crucial in pain nursing care plans. These goals are tailored to individual needs‚ ensuring realistic expectations for pain relief and functional improvement. Nurses use baseline assessments to establish specific‚ achievable objectives‚ such as reducing pain intensity or improving mobility. Goals are framed using SMART criteria: Specific‚ Measurable‚ Achievable‚ Relevant‚ and Time-bound. For example‚ a goal might be “The patient will report a pain level of 3/10 within 48 hours.” Regular documentation and evaluation ensure progress tracking and adjustments as needed. Patient involvement in goal-setting fosters engagement and adherence to care plans‚ promoting better outcomes and enhanced quality of life.
4.2 Short-Term Goals for Pain Relief
Short-term goals for pain relief are designed to address immediate discomfort and improve patient comfort within a 24- to 72-hour timeframe. These goals focus on reducing pain intensity‚ enhancing mobility‚ and minimizing distress. Examples include achieving a pain level of 4/10 or below on the numerical rating scale or demonstrating improved ability to perform daily activities. Interventions such as pharmacological therapies‚ relaxation techniques‚ or positional adjustments are often implemented to meet these objectives. Regular assessments ensure progress toward these goals‚ allowing nurses to adjust care plans as needed. Measurable outcomes‚ such as reduced pain reports or increased participation in care‚ validate the effectiveness of interventions and guide further adjustments for optimal relief.
4.3 Long-Term Goals for Pain Management
Long-term goals for pain management focus on improving the patient’s overall quality of life and functional abilities. These goals are typically achieved over weeks to months and emphasize sustainable pain control. Objectives may include reducing reliance on pain medications‚ enhancing physical mobility‚ and promoting psychological well-being. Patient education plays a key role‚ teaching individuals to manage pain independently through techniques like relaxation exercises and lifestyle modifications. Non-pharmacological interventions‚ such as therapy or alternative therapies‚ are often integrated into long-term plans. Regular follow-ups and adjustments to care ensure continued progress. The ultimate aim is to empower patients to lead fulfilling lives despite chronic pain‚ fostering independence and resilience through personalized care strategies.

Nursing Interventions for Pain Management
Nursing interventions for pain management are tailored to address both acute and chronic pain effectively. Pharmacological interventions include administering prescribed analgesics‚ such as opioids or NSAIDs‚ while monitoring for side effects. Non-pharmacological approaches‚ like relaxation techniques‚ breathing exercises‚ and guided imagery‚ help reduce discomfort without medication. Nurses also employ physical modalities‚ such as heat or cold therapy‚ to alleviate pain. Patient education is crucial‚ teaching individuals about pain management strategies and proper medication use. Additionally‚ nurses encourage activities that promote comfort and distraction‚ such as music therapy or mindfulness practices. These interventions are adjusted based on patient responses‚ ensuring personalized and holistic care that addresses physical‚ emotional‚ and psychological needs to enhance overall well-being.
5.1 Pharmacological Interventions for Pain Relief
Pharmacological interventions are a cornerstone of pain management‚ offering effective relief for both acute and chronic pain. Nurses administer analgesics‚ such as NSAIDs‚ opioids‚ and acetaminophen‚ tailored to the patient’s condition and pain severity. These medications are often prescribed in a stepwise approach‚ starting with milder options and progressing to stronger drugs as needed. Patient education is crucial to ensure safe use‚ proper dosing‚ and awareness of potential side effects. Nurses also monitor for adverse reactions‚ such as respiratory depression or constipation‚ especially with opioid use. Adjustments to the pharmacological regimen are made based on patient feedback and pain assessment outcomes‚ ensuring optimal relief while minimizing risks. This approach aligns with individualized care plans‚ promoting comfort and improving quality of life.
5.2 Non-Pharmacological Interventions and Techniques
Non-pharmacological interventions are vital in pain management‚ offering patients alternative methods to alleviate discomfort without medication. Techniques such as relaxation exercises‚ deep breathing‚ and guided imagery help reduce stress and promote relaxation. Distraction methods‚ like music therapy or mindfulness‚ divert the patient’s focus away from pain. Additionally‚ physical modalities such as heat or cold therapy can reduce inflammation and discomfort. Nurses also encourage activities like yoga or gentle stretching to improve mobility and mood. These methods are often combined with pharmacological interventions to enhance pain relief. Patient education on these techniques empowers individuals to take an active role in managing their pain. Non-pharmacological approaches are particularly beneficial for patients with contraindications to certain medications or those seeking holistic care options.
5.3 Relaxation and Breathing Exercises for Pain Control
Relaxation and breathing exercises are effective non-pharmacological interventions for pain control. Techniques like deep breathing‚ guided imagery‚ and progressive muscle relaxation help reduce tension and discomfort. These methods encourage patients to focus on calming their minds and bodies‚ diverting attention from pain. Breathing exercises‚ such as diaphragmatic breathing‚ can slow heart rates and lower stress hormones‚ promoting relaxation. Nurses often incorporate these exercises into care plans‚ teaching patients how to practice them independently. Regular use of these techniques can enhance pain tolerance and improve overall well-being. By including relaxation exercises in pain management plans‚ nurses provide patients with empowering tools to cope with discomfort and regain control over their pain experience.

Evaluation of Pain Management Outcomes
Evaluation of pain management outcomes involves assessing pain relief‚ functional improvement‚ and patient satisfaction. Regular monitoring ensures interventions are effective and guides adjustments to care plans as needed.
6.1 Measuring the Effectiveness of Pain Interventions
Evaluating the effectiveness of pain interventions requires consistent assessment and documentation. Nurses use pain scales and patient feedback to measure progress. Behavioral cues‚ functional ability‚ and reduced pain intensity indicate successful outcomes. Regular follow-ups ensure interventions are adjusted based on patient response; Accurate documentation helps track improvements and guides future care decisions. Effective measurement ensures personalized and evidence-based approaches‚ enhancing patient satisfaction and recovery. This process is crucial for refining care plans and achieving desired pain management goals.
6.2 Patient Feedback and Satisfaction Assessment
Patient feedback is crucial for evaluating the effectiveness of pain management strategies. Nurses use surveys‚ interviews‚ or verbal assessments to gather insights into the patient’s experience. This feedback helps determine if interventions are meeting the patient’s needs and improving their quality of life. Satisfaction assessment also identifies areas for improvement in care delivery. By incorporating patient perspectives‚ nurses can refine pain care plans to better address individual preferences and expectations. Regular feedback collection ensures that pain management remains patient-centered and aligned with desired outcomes. This collaborative approach fosters trust and enhances the overall effectiveness of care. Patient satisfaction is a key indicator of successful pain management interventions.

6.3 Documentation of Pain Relief Progress
Accurate and consistent documentation of pain relief progress is vital for tracking patient outcomes and informing care decisions. Nurses record changes in pain intensity‚ patient-reported relief‚ and the effectiveness of interventions. This documentation includes objective data‚ such as pain scores‚ and subjective feedback from the patient. Regular updates ensure continuity of care and help identify patterns or areas needing adjustment. Using standardized tools‚ like PDF templates‚ enhances clarity and consistency in reporting. Timely documentation also supports legal and ethical standards‚ providing a clear record of care provided. By maintaining detailed records‚ healthcare teams can evaluate the effectiveness of pain management strategies and make data-driven decisions to improve patient care. This process ensures transparency and accountability in pain relief efforts.

Patient Education in Pain Nursing Care
Patient education empowers individuals to manage pain effectively through tailored strategies‚ encouraging self-care techniques‚ and adherence to prescribed regimens‚ enhancing overall well-being and recovery.
7.1 Teaching Patients About Pain Management Strategies
Teaching patients about pain management strategies is crucial for empowering them to take an active role in their care. Nurses should educate patients on various techniques such as deep breathing exercises‚ progressive muscle relaxation‚ and guided imagery to help alleviate pain. Additionally‚ patients should be informed about the use of non-pharmacological methods like heat therapy‚ cold therapy‚ and music therapy. Providing patients with resources‚ such as pain management guides or customizable PDF templates‚ can enhance their understanding and adherence to prescribed regimens. By fostering patient education‚ nurses enable individuals to better manage their pain‚ reduce discomfort‚ and improve their overall quality of life. This educational process is a cornerstone of holistic pain care.
7.2 Encouraging Comfort Measures and Distraction Techniques
Encouraging comfort measures and distraction techniques is vital for enhancing patient comfort and reducing pain perception. Nurses can guide patients in using relaxation methods such as deep breathing exercises‚ guided imagery‚ and music therapy to create a calming environment. Distraction techniques like mindfulness‚ reading‚ or listening to soothing music can divert the patient’s focus away from pain. Comfort measures‚ such as adjusting the room temperature or providing pillows for support‚ can also contribute to a more soothing experience. By integrating these strategies into pain care plans‚ nurses help patients manage discomfort more effectively‚ improving their overall well-being and quality of life. These techniques are often included in customizable PDF templates for consistency and ease of implementation.
7.3 Promoting Adherence to Prescribed Pain Regimens
Promoting adherence to prescribed pain regimens is crucial for effective pain management. Nurses play a key role in educating patients about the importance of following their treatment plans‚ including medication schedules and non-pharmacological interventions. Clear communication and setting realistic expectations help patients understand their roles in managing pain. Simplifying medication regimens and providing written instructions can improve compliance. Encouraging patients to track their pain levels and responses to treatments fosters accountability and engagement. Positive reinforcement and addressing potential barriers‚ such as fear of addiction or side effects‚ can also enhance adherence. Regular follow-ups and adjustments to the plan ensure sustained commitment‚ ultimately improving patient outcomes and quality of life. Customizable PDF templates can aid in documenting and guiding these efforts consistently.

Documentation and Reporting in Pain Care Plans
Accurate documentation ensures continuity of care‚ legal compliance‚ and effective communication. Using PDF templates standardizes reporting‚ maintaining consistency and clarity in pain assessment and intervention records.
8.1 Maintaining Accurate Records of Pain Assessment
Maintaining accurate records of pain assessment is crucial for effective care. Detailed documentation ensures continuity‚ legal compliance‚ and clear communication between healthcare providers. PDF templates provide structured formats‚ capturing subjective and objective data‚ such as pain intensity‚ location‚ and duration. These records help track progress‚ identify trends‚ and guide future interventions. Regular updates ensure that patient needs are consistently met‚ fostering a coordinated approach to pain management. Accurate documentation also supports accountability and informed decision-making‚ ultimately improving patient outcomes and satisfaction. By using standardized templates‚ nurses can efficiently document assessments‚ ensuring comprehensive and reliable records that align with best practices in pain care.
8.2 Legal and Ethical Considerations in Documentation
Legal and ethical considerations are paramount in pain documentation. Accuracy and transparency ensure patient trust and protect nurses from liability. Detailed‚ objective records comply with regulations and safeguard confidentiality. Ethical practice demands respect for patient autonomy‚ with clear communication about documentation purposes. Adhering to professional standards prevents errors and misinterpretations. PDF templates guide structured‚ unbiased reporting‚ minimizing legal risks. Proper documentation also supports continuity of care and accountability. Nurses must avoid subjective interpretations and ensure data reflects patient-centered care. Ethical documentation upholds professionalism‚ fosters trust‚ and aligns with legal requirements‚ ensuring high-quality patient outcomes and adherence to healthcare standards. Compliance with these principles is essential for maintaining integrity in pain care documentation.
8.3 Using PDF Templates for Consistent Reporting
PDF templates streamline pain care documentation‚ ensuring consistency and organization. They provide structured formats for recording patient assessments‚ goals‚ and interventions‚ reducing variability. Pre-designed sections for subjective and objective data‚ diagnoses‚ and outcomes simplify the reporting process. Templates promote standardization across care teams‚ improving communication and continuity. They also include placeholders for patient-specific details‚ ensuring personalized care plans. Easy to download and customize‚ PDF templates save time and reduce errors. They often include examples and guidelines‚ making them user-friendly for nurses. Consistent reporting enhances clarity and accountability‚ benefiting both patients and healthcare providers. By using PDF templates‚ nurses can efficiently document care plans‚ ensuring comprehensive and uniform patient records. This fosters better collaboration and adherence to best practices in pain management.
PDF templates ensure uniformity in documenting pain care plans‚ simplifying the reporting process. They provide structured formats for assessments‚ goals‚ and interventions‚ reducing variability and enhancing clarity. These templates include sections for subjective and objective data‚ diagnoses‚ and outcomes‚ making it easier to track progress. Healthcare providers can customize them to meet specific patient needs while maintaining consistency. PDF templates also save time‚ minimize errors‚ and promote standardization across care teams. They often include examples and guidelines‚ guiding nurses in creating comprehensive and organized care plans. By using PDF templates‚ nurses can efficiently document patient care‚ ensuring accurate and consistent reporting that supports better patient outcomes and collaboration.
9.1 Reviewing the Effectiveness of Pain Care Plans
Regularly reviewing pain care plans ensures their effectiveness in addressing patient needs. This involves evaluating outcomes‚ such as pain relief‚ functional improvement‚ and patient satisfaction. Nurses assess whether goals are met using tools like pain scales and patient feedback. Documentation plays a key role in tracking progress and identifying areas for adjustment. PDF templates help maintain consistency in reporting‚ allowing for clear comparisons over time. Effective reviews enable nurses to refine interventions‚ ensuring personalized and evidence-based care. Continuous evaluation supports better patient outcomes and aligns with a patient-centered approach to pain management. By reviewing care plans‚ nurses can adapt strategies to meet evolving patient needs‚ fostering improved quality of life and holistic well-being.
9.2 Updating Nursing Care Plans Based on Patient Feedback
Patient feedback is crucial for refining nursing care plans‚ ensuring they remain relevant and effective. Nurses gather insights through surveys‚ interviews‚ or direct communication‚ identifying what aspects of the plan are beneficial or require adjustment. This feedback loop allows for timely modifications to goals‚ interventions‚ and outcomes‚ enhancing patient satisfaction and care quality. By incorporating feedback‚ nurses can address unmet needs‚ improve pain management strategies‚ and align care with patient preferences. PDF templates facilitate seamless updates‚ maintaining consistency and clarity in documentation. Regular updates based on patient input foster a collaborative care environment‚ promoting better outcomes and continuous improvement in pain management. This iterative process underscores the importance of patient-centered care in nursing practice.
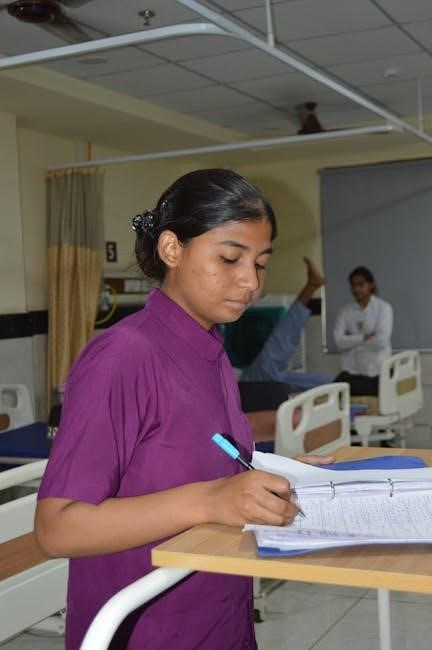
9.3 The Role of Nurses in Holistic Pain Management
Nurses play a pivotal role in holistic pain management by addressing the physical‚ emotional‚ and psychological aspects of pain. They assess patients’ unique needs‚ develop personalized care plans‚ and implement evidence-based interventions. Nurses educate patients and families about pain management strategies‚ including pharmacological and non-pharmacological approaches. By advocating for patients’ preferences and promoting comfort measures‚ nurses empower individuals to take an active role in their care. Their ability to provide emotional support and address existential concerns further enhances the holistic approach. Utilizing PDF templates for care plans ensures consistency and organization‚ enabling nurses to deliver comprehensive‚ patient-centered care effectively. This holistic perspective underscores the nurse’s role as a key advocate for optimal pain relief and improved quality of life.